SlowItDownCKD
Best Six Kidney Disease Blogs of 2016 & 2017; winner Top 75 Nephrology Blogs
James’s Kidney Transplant Wasn’t Preemptive
 Last week, the third week of National Kidney Month, Kevin Fowler told us his story of the journey to his preemptive kidney transplant. This week, the fourth of National Kidney Month, James will tell us of his journey to a non preemptive kidney transplant. In case you were wondering, James and I met at an AAKP meeting in Tampa several years ago and just never lost contact. But let’s allow Uncle Jim (as he prefers to be called) tell his story.
Last week, the third week of National Kidney Month, Kevin Fowler told us his story of the journey to his preemptive kidney transplant. This week, the fourth of National Kidney Month, James will tell us of his journey to a non preemptive kidney transplant. In case you were wondering, James and I met at an AAKP meeting in Tampa several years ago and just never lost contact. But let’s allow Uncle Jim (as he prefers to be called) tell his story.
My name is James Myers. I live in Hammond, IN. I am an ESRD & PKD patient. I was lucky enough to have a transplant on April 27th, 2016. I write to you today to tell you my story, as well as my experiences with polycystic kidney disease. At the age of 25, I went into the hospital with chest pain. From a simple x-ray, I was diagnosed with PKD.
I have lost five members of my family to PKD, including my dad. Because of my family’s history, I was immediately referred to Dr. Hellman, a nephrologist at Indiana University Health. He promptly put me on high blood pressure medication and a renal diet. I faithfully followed up at the kidney clinic every six months and took my medicine. I did the best I could do to stay on the kidney diet. There is no cure for PKD, and at that time, there was very little they could do for me.
I tried to ignore my condition and carry on with my life, but in reality, the fact is that after I was diagnosed with kidney failure, all of my decisions were colored by my impending death, or so I thought. It was a factor in a failed marriage, a legal career being cut short, and two professorships at two different colleges lost. I loved being with the kids.
or so I thought. It was a factor in a failed marriage, a legal career being cut short, and two professorships at two different colleges lost. I loved being with the kids.
 or so I thought. It was a factor in a failed marriage, a legal career being cut short, and two professorships at two different colleges lost. I loved being with the kids.
or so I thought. It was a factor in a failed marriage, a legal career being cut short, and two professorships at two different colleges lost. I loved being with the kids.
Every step that I took from the date of my diagnosis was for one reason and one reason only; to avoid dialysis. I was able to do that for over 30 years, but in 2012. I could not delay it any longer. I began passing out, at home, in my classroom, everywhere. Many times after passing out, I was fearful I would be unable to reach the phone and call for help. I lived alone, and this caused a great deal of anxiety. At the age of 58, on July 28th, I started what would be a four year stretch on dialysis. My schedule was three days a week, four hours per session.
I was very, very angry when I first went on dialysis. After watching my dad die, I felt this was the beginning of the end. I had dreaded this for a long time. My dad passed after a short five years on dialysis, and I felt I was on the same life path as he. My days were numbered. I observed that many of my clinic mates came to the center by ambulance, were brought in on a gurney, walker, or wheelchair. Many used a cane. Many were diabetic on top of ESRD, and had suffered amputations. Five people were 90 years old or more. One woman was autistic and had the mentality of a 10 year old.
One of my dearest friends, Maureen O’Brien, looked after me. She forced me to open my eyes. I was able to drive and walk around on my own power. I had a fairly clear mind. I was taking classes toward two MBAs and was teaching other MBA candidates at the same time. Maureen had been dealing with kidney disease since the age of six. Every step along the way she had to argue and fight with healthcare officials. She had three transplants. Maureen provided encouragement and a bright, vivid smile. She provided a light on my path.
I began to understand my role. I made a conscious choice. I wanted to help my fellow Kidney Patients. I wanted to use my loud voice to help others. I wanted to advocate for my clinic mates who could not advocate for themselves. I did not like the way the dialysis clinics, the government, and the care staff pushed around or neglected my fellow Kidney Patients. The last straw for me was when they began to push for the cutting of funds to dialysis patients and clinics. I looked around the room and I realized with my health and skill set, I was the only one who could help. It occurred to me that if i did not accept this responsibility, maybe no one else would.
I joined as many kidney organizations as I could, I applied to be an advocate for as many groups as I could. I became very, very active on social media. I wrote petitions, I blogged, I contacted newspapers, I spoke and visited with my Congressman and Senators. I spoke frequently. To this day, I do whatever I have to do to bring about change for my fellow Kidney Patients. My life has purpose now. I like to think that my dad & Maureen would be proud of me.
I know that many of you are not used to me writing this way. I feel it is my responsibility to lift spirits, so I rarely talk about personal issues anymore. It is my hope to inspire others to likewise advocate for our fellow Kidney Patients. My friend Gail asked me to write my story out. Gail has been very candid with me, so I felt as she advocates for us, I should be just as candid with her & all of you. The point of this Kidney Story is to raise hope and to thank Gail and all of you that advocate for Kidney Patients.
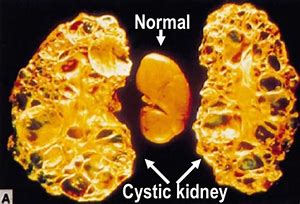 PKD affects approximately 600, 000 Americans and 12.5 million people worldwide. It is one of the most inherited diseases on the planet. Polycystic Kidney Disease is more common than Cystic Fibrosis, Sickle Cell Anemia, Muscular Dystrophy, Hemophilia, Downs Syndrome, and Hodgkins Disease combined. PKD is one of the four leading causes of Kidney Failure. It costs the federal government in excess of $2 Billion annually in Medicare and Medicaid costs for dialysis, transportation and related treatment. There is no cure.
PKD affects approximately 600, 000 Americans and 12.5 million people worldwide. It is one of the most inherited diseases on the planet. Polycystic Kidney Disease is more common than Cystic Fibrosis, Sickle Cell Anemia, Muscular Dystrophy, Hemophilia, Downs Syndrome, and Hodgkins Disease combined. PKD is one of the four leading causes of Kidney Failure. It costs the federal government in excess of $2 Billion annually in Medicare and Medicaid costs for dialysis, transportation and related treatment. There is no cure.
Sincerely,
James Myers
2019 Advocate of the Year for the NKF
BOD and Ambassador for the AAKP
Ambassador for the Chronic Disease Coalition
Ambassador for the NKF of Indiana
Ambassador for the American Kidney Fund
Ambassador for the PKD Foundation
Ambassador for the DPC
2019 Advocate of the Year for the NKF
BOD and Ambassador for the AAKP
Ambassador for the Chronic Disease Coalition
Ambassador for the NKF of Indiana
Ambassador for the American Kidney Fund
Ambassador for the PKD Foundation
Ambassador for the DPC

Thank you, Uncle Jim, for your generous sharing and even more generous advocacy.
Until next week,
Keep living your life!
Kevin Got His Preemptive Kidney Transplant
 Several years ago, I was invited to a kidney disease meeting. That’s where I first met Kevin Fowler, Principal of The Voice of the Patient, Inc. I liked listening to his ideas. Later, we walked into each other at an AAKP conference. This time I thoroughly enjoyed his company, but had quite a few questions about pre-emptive transplants. Kevin was good enough to explain his story, which answers my questions, in this guest blog during National Kidney Month. Take it away, Kevin!
Several years ago, I was invited to a kidney disease meeting. That’s where I first met Kevin Fowler, Principal of The Voice of the Patient, Inc. I liked listening to his ideas. Later, we walked into each other at an AAKP conference. This time I thoroughly enjoyed his company, but had quite a few questions about pre-emptive transplants. Kevin was good enough to explain his story, which answers my questions, in this guest blog during National Kidney Month. Take it away, Kevin!
Kidney disease has always been a part of my life. When I was growing up, my mom told me stories about her father who had suffered from Autosomal Polycystic Kidney Disease ( ADPKD), a disease which prompts the growth of cysts on the kidneys. My mom was the oldest of three sisters, and had great love and affection for my grandfather, Hubert Duvall. I never had a chance to meet him because he died before I was born. It was the late 1950s when he was admitted to the hospital because he was not feeling well. Unknown to him, he was experiencing uremia, the inability of the kidneys to rid themselves of waste products such as urea, as he went into kidney failure. Shortly after his hospital admission he died. As he neared death, he learned that ADPKD was the cause of his kidney failure.
My grandfather’s patient journey had a profound impact upon his three daughters: Mary Ann, Ruth, and Laverne in that his genetic disease was passed on to each of them. My mom, Mary Ann, was diagnosed after the birth of her third child. Imagine the joy of giving birth to a child while being diagnosed with a disease with limited scientific knowledge and a very uncertain future. My mom and dad faced the unknown with a positive attitude, but with very little professional guidance.
As a young boy, I was very close to my mom. I felt her unconditional love for me, and her whole life was dedicated to her three children. As her ADPKD advanced, I saw her suffer with the disease. I saw her experience constant back pain, routine exhaustion and nausea. All of this physical suffering was difficult to understand as a young child. Moreover, what was really difficult was the look on her face as she faced a nebulous future.
Eventually, my mom’s kidneys failed. Unlike my grandfather, hemodialysis was available as a treatment option to sustain her life. She started hemodialysis at the age of 48. While she approached dialysis with optimism, her future was never clear to her or our family. I saw my mom struggle to survive on dialysis. I saw her return home from dialysis feeling exhausted and tired. I saw that when she had a rough hemodialysis session, it would take her longer to recover from the treatment. She never bemoaned her fate, and provided us the legacy of her example.
After four and a half years on hemodialysis, my mom died at the age of 52. Her dialysis experience left an indelible impression upon me. From that point on, I lived in fear that I would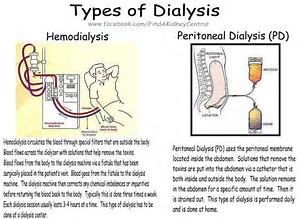 face the same fate. I choose to never determine if I had the same disease. In many ways, it was a rational decision. Interventions were not able to slow down the progression of ADPKD. If I were diagnosed with ADPKD, I would be penalized. I would face difficulty obtaining health and life insurance. The fear of facing the same patient journey as my mom was always hanging over my head, and I didn’t have the courage to determine if I too had ADPKD.
face the same fate. I choose to never determine if I had the same disease. In many ways, it was a rational decision. Interventions were not able to slow down the progression of ADPKD. If I were diagnosed with ADPKD, I would be penalized. I would face difficulty obtaining health and life insurance. The fear of facing the same patient journey as my mom was always hanging over my head, and I didn’t have the courage to determine if I too had ADPKD.
 face the same fate. I choose to never determine if I had the same disease. In many ways, it was a rational decision. Interventions were not able to slow down the progression of ADPKD. If I were diagnosed with ADPKD, I would be penalized. I would face difficulty obtaining health and life insurance. The fear of facing the same patient journey as my mom was always hanging over my head, and I didn’t have the courage to determine if I too had ADPKD.
face the same fate. I choose to never determine if I had the same disease. In many ways, it was a rational decision. Interventions were not able to slow down the progression of ADPKD. If I were diagnosed with ADPKD, I would be penalized. I would face difficulty obtaining health and life insurance. The fear of facing the same patient journey as my mom was always hanging over my head, and I didn’t have the courage to determine if I too had ADPKD.
I was married to my wife, Kathy, in 1995, and in less than five years we had two children. During this time, I was being seen by a primary care physician who was aware of my ADPKD family history. My kidney function was tested on my annual appointments, and he told me that my kidney function was fine. He stated that if I had ADPKD, there was not much that could be done to slow down the progression. Later that same year near the Christmas season, I experienced deep flank (the side of your body between the bottom rib and the hip) pain. Initially, I attributed it to moving some furniture. The pain persisted, and because of my additional responsibilities as a husband and father, I called my primary care physician requesting an ultrasound test. The ultrasound test would determine once and for all whether I too had ADPKD.
On a cold and sunny day in January 2001, my physician administered the ultrasound test. Watching his reaction told me all I needed to know. At the age of 39, I was informed that I would be in kidney failure within the next three to five years. He offered to make a nephrology referral, but I declined. Since he had not demonstrated competence managing my condition, I intuitively sensed that I could not trust his referral would serve my best interests.
 At that time, I was working in the pharmaceutical industry, so I called a physician friend at Barnes Hospital in St. Louis seeking a nephrology recommendation. On my mother’s birthday, I met with my nephrologist – who had a profound impact on my life. He informed me that it was not necessary to be on dialysis, and that I could have a preemptive kidney transplant. Because of my fear, I had never taken the time to learn about the different End Stage Kidney Disease treatment options. I was incredibly fortunate to receive the best treatment option.
At that time, I was working in the pharmaceutical industry, so I called a physician friend at Barnes Hospital in St. Louis seeking a nephrology recommendation. On my mother’s birthday, I met with my nephrologist – who had a profound impact on my life. He informed me that it was not necessary to be on dialysis, and that I could have a preemptive kidney transplant. Because of my fear, I had never taken the time to learn about the different End Stage Kidney Disease treatment options. I was incredibly fortunate to receive the best treatment option.
On this recently past World Kidney Day, the theme was prevention due to detection. In the United States approximately 90% of those with Stage 3 Chronic Kidney Disease are unaware of their condition. This is no longer acceptable. The American Kidney Health Executive Order has initiated a public campaign to detect kidney disease earlier. In fact, the National Kidney Foundation and CVS Kidney Care launched their public awareness campaign this month, National Kidney Month. Unlike when I was diagnosed, there are now approved treatments to slow down the progression of kidney diseases. There are potentially additional treatments in the pipeline for ADPKD, Diabetic Kidney Disease, FSGS, IGAN, etc. For many people there is no longer a need to live in fear. There is a very real possibility that their patient journey may change for the better.

Thank you, Kevin, for sharing your personal kidney journey with us. Kevin may be reached via email at kevinjohnfowler@gmail.com or on Twitter as @gratefull080504.
Until next week,
Keep living your life!
Missing the Connection
During this second week of National Kidney Month, we have another reader directed blog. She had stumbled across The Long Awaited Sulfa Blog and had some questions about it and NAC. Hold on, I’ll get to NAC in a moment. Let’s start with sulfite, which I had always thought was not the same as sulfa. Did our reader mistype? Her verbatim question was, “Have you heard anything about NAC and CKD with sulfite sensitivity?”

According to MedicineNet at https://www.medicinenet.com/script/main/art.asp?articlekey=27721:
“Sulfite sensitivity: Adverse reactions of an allergic nature to sulfites. Sulfites occur in fermentation and also occur naturally in a number of foods and beverages including wine. Sulfites are used for their preservative properties. Sulfite sensitivity occurs most often in asthmatic adults — predominantly women. It is uncommon in preschool children. Adverse reactions to sulfites in nonasthmatics are rare. Sulfite sensitivity reactions range from mild to severe and may include skin, respiratory, or gastrointestinal signs and symptoms. Bronchoconstriction with wheezing is the most common sensitivity response in asthmatics.”
While I do know this reader is a woman, I do not know if she is asthmatic or a wine drinker.
Let’s move along to NAC. Healthline at https://www.healthline.com/nutrition/nac-benefits#section12 (Yes, that is the same Healthline that chose SlowItDownCKD as best kidney blog two years in a row.) tells us, it is N-Acetyl Cysteine and explains what this supplement is and what it can do for you. I added asterisks next to definitions you may need.
“Cysteine is a semi-essential amino acid.
It’s considered semi-essential because your body can produce it from other amino acids, namely methionine and serine. It becomes essential only when the dietary intake of methionine and serine is low.
Cysteine is found in most high-protein foods, such as chicken, turkey, yogurt, cheese, eggs, sunflower seeds and legumes.
N-acetyl cysteine (NAC) is a supplement form of cysteine.
Consuming adequate cysteine and NAC is important for a variety of health reasons — including replenishing the most powerful antioxidant in your body, glutathione. These amino acids also help with chronic respiratory conditions, fertility and brain health.
Here are the top 9 health benefits of NAC.
- Essential for Making the Powerful Antioxidant Glutathione
NAC is valued primarily for its role in antioxidant production.
Along with two other amino acids — glutamine and glycine — NAC is needed to make and replenish glutathione.
 *Glutathione is one of the body’s most important antioxidants, which helps neutralize free radicals that can damage cells and tissues in your body.
*Glutathione is one of the body’s most important antioxidants, which helps neutralize free radicals that can damage cells and tissues in your body.
It’s essential for immune health and fighting cellular damage. Some researchers believe it may even contribute to longevity ….
Its antioxidant properties are also important for combatting numerous other ailments caused by oxidative stress, such as heart disease, infertility and some psychiatric conditions….
- Helps With Detoxification to Prevent or Diminish Kidney and Liver Damage
NAC plays an important role in your body’s detoxification process.
It can help prevent side effects of drugs and environmental toxins….
In fact, doctors regularly give intravenous (IV) NAC to people with an acetaminophen overdose to prevent or reduce kidney and liver damage ….
NAC also has applications for other liver diseases due to its antioxidant and anti-inflammatory benefits ….
- May Improve Psychiatric Disorders and Addictive Behavior
*NAC helps regulate levels of glutamate — the most important neurotransmitter in your brain….
While glutamate is required for normal brain action, excess glutamate paired with glutathione depletion can cause brain damage.
This may contribute to mental health conditions, such as bipolar disorder, schizophrenia, obsessive-compulsive disorder (OCD) and addictive behavior….
For people with bipolar disease and depression, NAC may help decrease symptoms and improve your overall ability to function. What’s more, research suggests that it may play a role in treating moderate to severe OCD ….
NAC supplements can also help decrease withdrawal symptoms and prevent relapse in cocaine addicts ….
- Helps Relieve Symptoms of Respiratory Conditions
NAC can relieve symptoms of respiratory conditions by acting as an antioxidant and expectorant, loosening mucus in your air passageways.
As an antioxidant, NAC helps replenish glutathione levels in your lungs and reduces inflammation in your bronchial tubes and lung tissue.
People with chronic obstructive pulmonary disease (COPD) experience long-term oxidative damage and inflammation of lung tissue, which causes airways to constrict — leading to shortness of breath and coughing.
NAC supplements have been used to improve COPD symptoms, exacerbations and lung decline ….
Those with chronic bronchitis can also benefit from NAC.
Bronchitis occurs when the mucous membranes in your lungs’ bronchial passageways become inflamed, swell and shut off airways to your lungs….
By thinning mucus in your bronchial tubes and boosting glutathione levels, NAC may help decrease the severity and frequency of wheezing, coughing and respiratory attacks ….
In addition to relieving COPD and bronchitis, NAC may improve other lung and respiratory tract conditions like cystic fibrosis, asthma and pulmonary fibrosis, as well as symptoms of nasal and sinus congestion due to allergies or infections ….
- Boosts Brain Health by Regulating Glutamate and Replenishing Glutathione
NAC’s ability to replenish glutathione and regulate brain glutamate levels can boost brain health.
*The brain neurotransmitter glutamate is involved in a broad range of learning, behavior and memory actions, while the antioxidant glutathione helps reduce oxidative damage to brain cells associated with aging….
Because NAC helps regulate glutamate levels and replenish glutathione, it may benefit those with brain and memory ailments ….
NAC supplements appear to improve both dopamine function and disease symptoms such as tremors ….
- May Improve Fertility in Both Men and Women
 Approximately 15% of all couples trying to conceive are affected by infertility. In almost half of these cases, male infertility is the main contributing factor ….
Approximately 15% of all couples trying to conceive are affected by infertility. In almost half of these cases, male infertility is the main contributing factor ….
Many male infertility issues increase when antioxidant levels are insufficient to combat free radical formation in your reproductive system. The oxidative stress can cause cell death and reduced fertility ….
In some cases, NAC has been shown to improve male fertility….
In addition, NAC may improve fertility in women with polycystic ovary syndrome (PCOS) by inducing or augmenting the ovulation cycle ….
- May Stabilize Blood Sugar By Decreasing Inflammation in Fat Cells
High blood sugar and obesity contribute to inflammation in fat tissue.
This can lead to damage or destruction of insulin receptors and put you at a higher risk of type 2 diabetes ….
- May Reduce Heart Disease Risk by Preventing Oxidative Damage
Oxidative damage to heart tissue often leads to heart disease, causing strokes, heart attacks and other serious conditions.
NAC may reduce heart disease risk by reducing oxidative damage to tissues in your heart ….
It has also been shown to increase nitric oxide production, which helps veins dilate and improves blood flow. This expedites blood transit back to your heart and can lower your risk of heart attacks ….
- Ability to Boost Glutathione Levels May Improve Immune Function
NAC and glutathione also boost immune health.
Research on certain diseases associated with NAC and glutathione deficiency suggests that immune function might be improved — and potentially restored — by supplementing with NAC….
High levels of NAC in your body may also suppress HIV-1 reproduction.
For your body to make the amino acid cysteine, you need adequate amounts of folate, vitamin B6 and vitamin B12. These nutrients can be found in beans, lentils, spinach, bananas, salmon and tuna.
While most protein-rich foods, such as chicken, turkey, yogurt, cheese, eggs, sunflower seeds and legumes, contain cysteine, some people choose to supplement with NAC to increase their cysteine intake.
NAC has low bioavailability as an oral supplement, meaning that it’s not well absorbed. The accepted daily supplement recommendation is 600–1,800 mg of NAC ….”

Okay, I don’t get it. Have I missed something about the connection between sulfite sensitivity and NAC? If you can find what I missed, please let us know.
Ah, if only I could have been more helpful.
Until next week,
Keep living your life!
Dax’s Journey to Dialysis Friendly Clothing
I met Dax Francis a few years ago in a Facebook CKD & Dialysis Support page. Slowly, I became aware that he produces dialysis clothing… and that fascinated me. Then it dawned on me that you should know such clothing exists, although Dax is not the only one who produces them. I asked him if he would write a guest blog explaining how this all started and where he got the idea. He promptly agreed and that will be today’s blog, the first blog in March, National Kidney Month.
Before we read Dx’s blog, some of us may need a reminder of what FSGS is. According to The Mayo Clinic at https://www.mayoclinic.org/diseases-conditions/fsgs/symptoms-causes/syc-20354693:
“Focal segmental glomerulosclerosis (FSGS) is a disease in which scar tissue develops on the parts of the kidneys that filter waste from the blood (glomeruli). FSGS can be caused by a variety of conditions.
FSGS is a serious condition that can lead to kidney failure, for which the only treatment options are dialysis or kidney transplant. Treatment options for FSGS depend on the type you have.”
 I think we’re ready for Dax’s guest blog now.
I think we’re ready for Dax’s guest blog now.
My name is Dax Francis. I was diagnosed with FSGS as a young man, age twelve, and it was as if overnight school, sports, and friends were replaced with doctors, hospitals, and treatments. I struggled to find my place in this new body that could no longer do the things that had defined my life. Shortly after I graduated from high school, I had to begin dialysis which set me down a dark path of loneliness, depression, and sadness.
When I began dialysis I wanted everything to end. This was not the life I had ever wanted, and I believed that all my abilities, my skills, and talents were hidden behind a treatment filled with pain. The strength it took to live in that struggle was too much, and I put myself in situations where everything could have and should have ended. I was lost, and then I got that call saying it was my turn for a kidney transplant.
This was it! This is my moment to start my life! And then FSGS recurred shortly after surgery, and I was never able to leave treatment.

Devastation, utter devastation. I could not let my donor down though and felt a need to try to pursue my life once more despite the struggle. I enrolled in school for Social Work. I wanted to use my experiences to help those who may be in similar situations as myself, and I found my calling. Being able to help others and learn from those with wholly different lives and experiences than mine was the greatest gift I could have ever been given.
As I had all but finished the Social Work program, I realized that I could not be the social worker that people deserved due to my health. Being on treatment three times a week made it difficult to find work, and I rarely felt well enough to continually work. I struggled with this, feeling like I was never going to have a way to be a part of the world and the community nor was a place for me or anyone like me. This fact made me feel worthless and I dropped out of college 6 credits shy of my degree, because I thought it was pointless.
I wandered, confused, and didn’t know how to be someone who could make a difference. The wisdom I had gained from fighting every day to survive, I felt, was something special and I just wanted someone to ask me what I had learned while living in the struggle that is chronic illness. I just wanted someone to take notice of my fight and my struggle and see the person who can make a difference because of it all.
After the passing of a close friend I needed to live for both of us and put myself out there where I met someone who changed my life. I met someone who saw my fight and helped me realize that all I had been through made me capable of so much. She believed in me when I couldn’t believe in myself, this enabled me to live a life that I had always dreamed of, and I was doing it all despite being on dialysis. I was able to meet the love of my life despite the struggle. It all started with putting my true self out there and not being afraid of being that true person sharing with light and love.
 I enrolled back in school and finished my 6 credits finally achieving my degree. During this time the world began to change. More and more negativity seemed to be seeping into my life and I found myself in a negative space despite having everything I wanted. I needed to make a change. At the end of 2017 I committed to being positive, uplifting and to helping others the way I can. I started making videos while I was actually on dialysis just to let others know that they were not alone and that they needed to continue their fight.
I enrolled back in school and finished my 6 credits finally achieving my degree. During this time the world began to change. More and more negativity seemed to be seeping into my life and I found myself in a negative space despite having everything I wanted. I needed to make a change. At the end of 2017 I committed to being positive, uplifting and to helping others the way I can. I started making videos while I was actually on dialysis just to let others know that they were not alone and that they needed to continue their fight.
The support I received from those first videos inspired me to do more with my talents and abilities and Ivye Wear was born on the morning of January 13, 2018. I wanted to provide comfort, warmth, and hope to the warriors fighting every day to survive, often with little recognition of the strength it takes to survive and live in that struggle. I wanted to provide a suit of armor for the warrior when they go into battle; whether it’s dialysis, chemotherapy, infusions, or something else entirely, and I designed comfortable, accessible clothing designed for a range of medical treatments, procedures, and devices. Sweats, Hoodies, and T-Shirts designed for warriors, by warriors. All of our clothes provide zipper access to the vital areas your caregivers need to perform treatment while you can stay warm and dignified.
I never want anyone to feel as if they don’t have a place in this world due to their illness or struggle, Ivye Wear was born to be a beacon of hope for all chronic illness patients. I believe that it is our experiences that give us the strength, wisdom, and patience to change the world.

Thank you, Dax, for your honesty and especially for the dialysis clothing.
Until next week,
Keep living your life!
Meatless Monday and the Rest of the Week, Too
Whoa, baby! Lots and lots of reader interaction lately. One reader even wrote me to thank me for a blog I wrote years ago about sulfa… and here I was wondering if my blogs were being helpful. Thank you all for letting me know they are.
Talking about my blogs being helpful, another reader needs help with her non-animal protein diet. As a child, my brothers and I were cooked meat meals whenever my dad could afford it. I remember Mom cooking lots of hamburgers. That was the first food I learned to cook. As I got older, I realized I didn’t like the fatty taste of meat nor how much it needed to be chewed, so I ate it less and less. Now, since my husband is a meat eater, we have it once a week. He knows I don’t like it, but he does. I eat as much of it as I can before giving the rest to him. It isn’t very much. I think I’m going to learn quite a bit for myself, as well as my reader, in writing today’s blog.
Oster, the makers of the blender I use, at https://www.oster.com/blog/archive/2014/october/5-fruits-and-veggies-that-pack-the-protein.html#?sortby=newest offers us this information:
 “1. Avocado
“1. Avocado Like tomatoes, avocados are fruits that are commonly thought of as vegetables. But regardless of how you categorize it, an avocado carries more protein than a glass of milk, about 4 grams according to the United States Department of Agriculture. Although some avoid this fruit because it has a relatively high fat and calorie content, it’s full of a variety of nutrients such as zinc, folic acid, potassium, fiber and healthy fats….
- Lentils
Legumes are the most protein-rich group of vegetables available. On average, legumes can offer closer to animal products than many other vegetables in how much protein they offer. Among legumes, lentils are one of the highest in protein with about 47 grams of protein per cup, the USDA noted. - Apricots
Either raw or dried apricots can add protein to your meals as well as sweetness, though there’s debate over whether fresh or dehydrated is better. Although a raw apricot has more protein, dried apricots have more protein per bite because they’re more compact. Either way, you can’t go wrong. It’s a tasty, sweet way to add protein to your yogurt, oatmeal or other dishes. The USDA explained that 1 cup of sliced apricots has more than 2 grams of protein. - Spinach
This tasty leafy green is well known for being nutritious, but did you know it has nearly 3 grams of protein per every 100 grams of spinach, according to the USDA? But eating 100 grams of raw spinach can be hard…. Spinach is also rich in vitamin B6, riboflavin, niacin, vitamin C, a variety of minerals, and has minimal calories and fat. - Soybeans
Soybeans pack a walloping 68 grams of protein per cup, according to the USDA. Eat them raw, steam them or roast them for a tasty, protein-filled meal that has more of the nutrient some types of meat [have]. Soybeans are legumes, and also have significant daily amounts of iron, fiber and vitamin K.”
Notice the sentence about potassium in 1. Avocado. Hmmm, do we need to limit or cut out any of these other foods according to the renal diet? I went to SFGATE at https://healthyeating.sfgate.com/lentils-harmful-kidneys-12272.html for some answers.

“Are Lentils Harmful to the Kidneys?
Written by Meg Campbell; Updated November 28, 2018
Lentils are nothing but good news for the average person. The small, disc-shaped legumes are a low-fat, cholesterol-free source of high-quality protein, complex carbohydrates and several vitamins and minerals. Lentils are considered a diabetic-friendly, heart-healthy food because their high fiber content promotes normal blood sugar and cholesterol levels. Because they’re also rich in potassium, phosphorus, purines and oxalate, however, lentils aren’t an ideal choice for people affected by chronic kidney problems….
Lentils don’t harm healthy kidneys, just as they don’t damage unhealthy kidneys. Rather, people with chronic kidney problems may need to watch their intake of lentils because their kidneys are less able to adequately process certain nutrients. If you have chronic kidney disease, ask your physician for a detailed diet plan. Eating the right foods can help slow the disease’s progressio